Cutting Medicine Down to Size
By Paul T. Menzel
Originally Published in 1992
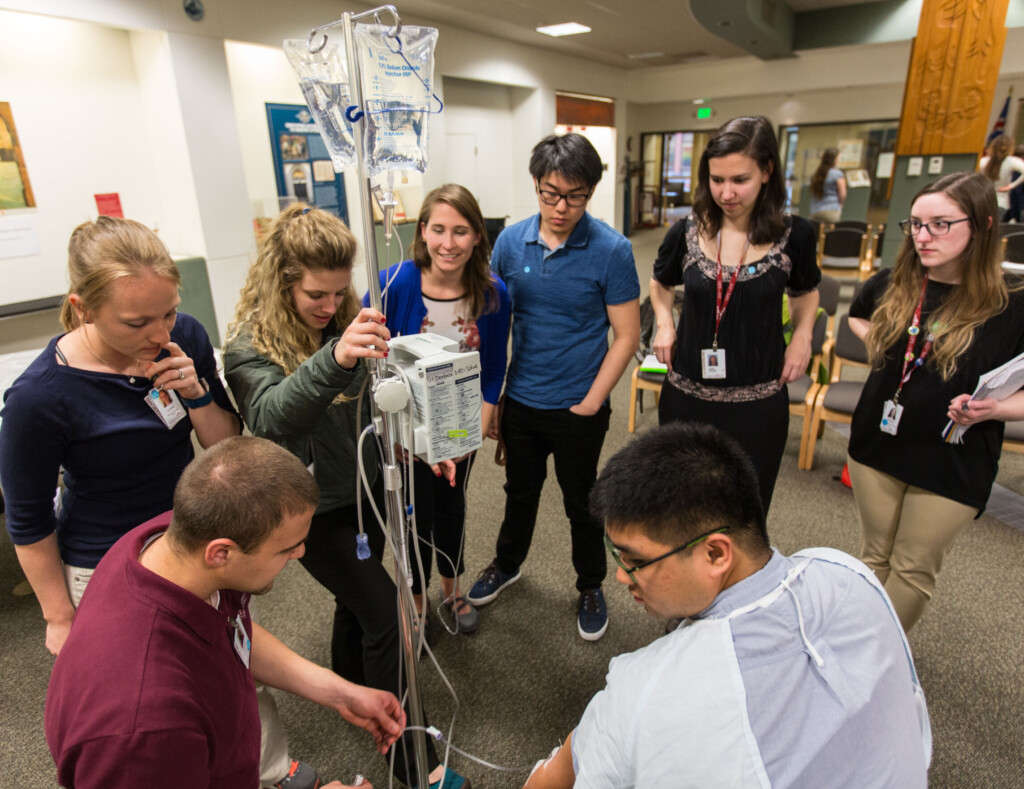
I thought I was used to medicine’s ever-expanding horizons, but I wasn’t prepared for this one. “We’ve got a dilemma we want some philosophers to help with,” said a pediatric endocrinologist on the other end of the line. As I quickly found out, for a long time now they have been treating very short children who have growth hormone deficiencies with injections of growth hormone [GH]. The treatments have been successful in many cases, adding to patients’ later height as adults. Until recently GH has been scarce, extracted from the pea-sized pituitary glands of cadavers. Now, however, Genentech, Inc. can manufacture it with recombinant DNA techniques, so there’s “plenty.” The treatments do cost $15,000 a year, of course, and usually they have to be administered for five years to make a difference, but GH is available.
“We don’t know what to do,” the physician went on. “We had no trouble previously drawing a line—we only used GH on very short kids with GH deficiency. Now some of us are beginning to treat non-GH-deficient, otherwise healthy, very short stature children, too. After all, they’re just as short, they often suffer as much from their stature handicap as the GH-deficient kids, and they can often gain as much extra height from GH treatments. Maybe we should treat everyone, say, in the shortest one percentile, or even others—a prospectively 5’4” Milton Friedman, say, could have been boosted to 5’7”. But where do we stop? Maybe we’ve already gone too far.”
I tried to grasp things more concretely. A 4’7” woman or a 5’1” man is in the lowest one percentile. (As I later learned, two of my faculty colleagues at PLU are in that category.) Treated with GH, whether they are naturally hormone-deficient or not, many will add three to four inches to their adult height. GH treatments have been proven to have no harmful physical side effects, though some critics believe that the regimen of thrice-a-week shots in the bum for years on end is only likely to exacerbate a child’s perceptions that shortness is a problem.
Indeed the pediatric specialists —only board certified endocrinologists— who are so far allowed access to GH by Genentech seem right in not viewing the “disease” of GH-deficiency as the relevant line. If a human need is served (or at least human “benefit” delivered) by adding three or four inches to the height of a likely very short person who’s GH-deficient, then a human need would also seem to be served by treating successfully a non-GH-deficient patient who is likely to be equally short. The ground for treating either at insurance company or public expense is the fact that their height can be a real handicap in the lives patients will lead.
We may desperately want “disease” to do the line-drawing trick for us here, but other than some crude distinction between serious diseases on the one hand and mere enhancements of appearance on the other (elective cosmetic surgery, for example), we have long ago stepped beyond diseases in our conception of the legitimate scope of basic medicine. Pregnancy, for example, is certainly a condition we should cover in public and private insurance, but it is only a condition that needs to be monitored, not a disease. We could, of course, call everything that we thought deserved medical treatment a “disease” just to save the belief that the only care we provide at collective expense is care to remedy the effects of disease, but then we would gain no substantive, policy-informing benefit from the concept. In the GH line-drawing controversy, we might as well call very short stature a disease from the start. Yet that’s laughable. It would certainly make more sense to call tall stature the disease; it causes us to build bigger cars and houses, for example, using up additional energy, space, and resources. The motto of the National Association of Short Adults (NASA), “Down in Front,” hits home.
Convinced that we are no longer armed with any potent notion of disease, where do we turn? Suppose we can further clarify the factual picture along these lines. We know ahead of time that certain conditions indicate potential for responding to GH treatment: not dwarfism, but a limited range of both GH-deficient and non-GH-deficient children. We can refine the pool of potentially benefitted children further, in turn, by dropping those who show no change in growth rate after a year or two of treatment. Among those on whom we then use full treatment, probably only three-fourths actually gain three inches or more in eventual adult height. In turn, of those three-fourths, it would seem a reasonable guess that half would not have experienced serious psychosocial adjustment problems because of their short stature anyway, and half would have. Of the latter, half in turn will find those problems largely unabated by a mere gain of three to four inches, and half will be significantly helped. That is, 25 percent of the 75 percent who gain height from long-term GH treatment will experience significant psychosocial gain. Thus, while five years of treatment costs “only” $75,000, each real adult height gain costs $100,000, and each major psychosocial gain costs $400,000.
As a parent, or physician, then, what should we do if our child or patient is prospectively very short? Though I can understand how pressures build up on us to desire every marginal improvement in opportunity that we can create, shouldn’t we also keep some perspective on what we are being pulled into here? For one thing, would we care about physical stature were it not for the influence of male-centered preconceptions about physical strength? And even then, will a gain of three or four inches much matter? Will the notion of a “handicapping height” – the lowest one percentile, for example, which is 4’7” and 5’1” respectively for women and men- begin to provide any kind of line? There will always be another bottom one percentile if we boost those who would only be 4’7” and 5’1”. As to equal opportunity in life, would we really choose to invest $75,000 in height-raising GH if we were truly intent on empowering the range of real opportunities for a child? Think of what a trust fund could later do for the child if that amount were truly invested. And what about other children who start from much greater total disadvantages and could be helped more with far fewer resources?
What is really tough for physicians and parents to notice at this point is that these considerations can apply to GH-deficient children as well. Even if they do have in some sense a biological “disease,” why should we think that warrants an investment of this magnitude when the benefits are as chancy and meager as they are? Instead of pushing us to expand GH treatment, our scepticism about the GH-deficiency line leads us back to criticism of what we have been doing even for so many GH-deficient children. Undoubtedly, some GH- (and non-GH-) deficient children do deserve help; Turner’s syndrome patients, for example, suffer a wide range of other handicaps and medical complications, and their gain in stature of close to half a foot from GH may constitute a significant increase in otherwise highly limited opportunities. But they are the exception, not the rule.
Am I wrong or insensitive in thinking that here is another case where we need to cut the narrow-sighted enthusiasm for a frontier technology down to size? Maybe we should say to medicine, “Down in front!”